NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Bookshelf ID: NBK351 PMID: 21250192
Definition
Cholesterol, triglycerides, and high-density lipoproteins are important constituents of the lipid fraction of the human body. Cholesterol is an unsaturated alcohol of the steroid family of compounds; it is essential for the normal function of all animal cells and is a fundamental element of their cell membranes. It is also a precursor of various critical substances such as adrenal and gonadal steroid hormones and bile acids. Triglycerides are fatty acid esters of glycerol and represent the main lipid component of dietary fat and fat depots of animals.Cholesterol and triglycerides, being nonpolar lipid substances (insoluble in water), need to be transported in the plasma associated with various lipoprotein particles. Plasma lipoproteins are separated by hydrated density; electrophretic mobility; size; and their relative content of cholesterol, triglycerides, and protein into five major classes: chylomicrons, very-low-density lipoproteins (VLDL), intermediate-density lipoproteins (IDL), low-density lipoproteins (LDL), and high-density lipoproteins (HDL).
Since the levels of plasma lipids have a bell-shaped distribution in the general population, the definition of either a high or a low value of these substances has remained an arbitrary statistical decision. High values have been traditionally considered as those in the 90th and 95th percentiles; low values were considered to be those below the 5th percentile. The NIH Concensus Conference has recently revised the values concerning cholesterol, however, in view of clear evidence of an increased risk of coronary atherosclerosis in persons falling in the 75th to 90th percentiles. According to this last statement, cholesterol levels below 200 mg/dl are classified as "desirable blood cholesterol," those 200 to 239 mg/dl as "borderline-high blood cholesterol," and those 240 mg/dl and above as "high blood cholesterol."
Technique
Analysis of plasma or serum total cholesterol, triglycerides, and lipoproteins is usually performed on blood specimens obtained by venipuncture in tubes containing EDTA. Because of a larger content of water, plasma levels have been found to be around 3% lower than matched serum levels. Cholesterol levels are fairly constant, but triglyceride levels fluctuate considerably from day to day and are highest 1 to 4 hours after meals.Collection of blood for triglyceride testing should be done after a 12-hour fasting period, when chylomicrons have ordinarily been cleared from the circulation. Measurements must be ideally done while the patients are on their usual diet and taking no medications that could alter blood lipid levels. Sampling should not be performed during periods of stress or within 6 weeks after a major illness, such as an acute myocardial infarction, as plasma cholesterol may be reduced and triglyceride levels increased in these instances.
The standard chemical determination for plasma cholesterol is the Abell-Kendall (A-K) technique, which involves the Liebermann-Burchardt reaction after hydrolysis and extraction of cholesterol. Samples for plasma cholesterol and triglyceride determinations are commonly analyzed by completely automated methods at clinical laboratories. As the results obtained at commercial laboratories differ systematically from those obtained by research methods, it is advisable to inquire how the method used by the particular laboratory compares with reference values, and to employ the same laboratory facility for serial measurements. The best reference values available today for North American populations are those obtained in the Lipid Research Clinics Program, which surveyed 12,595 Americans aged 20 to 79 in the United States and Canada. Reference values for plasma total cholesterol were obtained by utilizing autoanalyzer systems to which either the ferric chloride–sulfuric acid method or the Liebermann-Burchardt test was adapted. A fluorometric analysis was utilized to determine triglyceride reference values. Plasma high-density lipoprotein cholesterol (HDL-C) determination in this program was measured by the same procedures used for plasma total cholesterol, after precipitation of apoprotein B-containing lipoproteins in whole plasma (LDL and VLDL) by heparin–manganese chloride.
A useful additional test is examination of a refrigerated sample of fasting plasma at 4°C; chylomicrons, if present, form a creamy layer at the top of the test tube. This test could help to distinguish type 1 hyperlipoproteinemia (creamy layer on top with clear infranatant) from type 5 hyperlipoproteinemia (creamy layer on top with turbid infranatant).
Lipoproteins can be separated by ultracentrifugation, precipitation, and electrophoresis. Lipoprotein fractions can be quantified by preparative or density-adjusted ultracentrifugation. This method is usually employed in elaborate studies and not as a routine clinical tool. The quantitative reference method employs precipitation and ultracentrifugation sequentially to determine each lipoprotein component.
Usually, measurement of plasma lipid levels is sufficient for evaluation of patterns of lipoprotein elevations. Occasionally paper electrophoresis of the plasma is helpful. The correspondence of electrophoretic fractions with lipoproteins is shown in Table 31.1.
Quantitative determination of apoproteins is performed in sophisticated laboratories utilizing radioimmunoassays (for apoprotein AI and apoprotein B) and isoelectric focusing (for apoproteins C and E).
Other specialized tests are: (1) the intravenous heparin test for determination of postheparin lipolytic activity (this test measures the preheparin and postheparin liberation of lipoprotein lipase and is principally used to confirm congenital lipoprotein lipase deficiency), and (2) evaluation of LDL receptor status on cultured skin fibroblasts or isolated lymphocytes.
Basic Science
Plasma lipoprotein particles contain variable proportions of four major elements: cholesterol, triglycerides, phospholipids and specific proteins called apoproteins (Table 31.2). An alphabetical nomenclature (A, B, C, D, E.) is generally used to designate the apoproteins. The varying composition of these elements determines the density, size, and electrophoretic mobility of each particle. These factors in turn have been used for the clinical and biochemical classification of lipoprotein disorders. Schematically, lipoproteins have been described as globular or spherical units in which a nonpolar core lipid (consisting mainly of cholesterol esters and triglycerides) is surrounded by a layer containing phospholipids, apoproteins, and small amounts of unesterified cholesterol. Apoproteins, in addition to serving as carrier proteins, have other important functions such as being co-factors for enzymes involved in lipoprotein metabolism, acting as specific ligands for binding of the particles to cellular receptor sites, and intervening in the exchange of lipid constituents between lipoprotein particles.The fact that all the cholesterol required by the body can be produced by biosynthesis points to the essential nature of this substance. As an estimated loss of 1.0 to 1.5 g of cholesterol occurs daily through desquamation and fecal loss, this amount must be replaced. Usually this replacement is obtained from dietary sources, but another portion is synthesized in multiple cells of the body. Triglycerides are also obtained from the diet as well as synthesized by the liver.
The origin of circulating lipoproteins is less understood than is their uptake, transport, and degradation. The lipid transport system in plasma has been described as involving two pathways: an exogenous route for the transport of cholesterol and triglycerides absorbed from dietary fat in the intestine, and an endogenous system through which cholesterol and triglycerides reach the plasma from the liver and other nonintestinal tissues (Figure 31.1).
Exogenous Pathway
The exogenous pathway starts with the intestinal absorption of triglycerides and cholesterol from dietary sources. Its end result is the transfer of triglycerides to adipose and muscle tissue and of cholesterol to the liver. After absorption, triglycerides and cholesterol are re-esterified in the intestinal mucosal cells and then coupled with various apoproteins, phospholipids, and unesterified cholesterol into lipoprotein particles called chylomicrons. The chylomicrons in turn are secreted into intestinal lymph, enter the bloodstream through the thoracic: duct, and bind to the wall of capillaries in adipose and skeletal muscle tissue. At these binding sites the chylomicrons interact with the enzyme lipoprotein lipase, which causes hydrolysis of the triglyceride core and liberation of free fatty acids. These fatty acids then pass through the capillary endothelial cells and reach the adipocytes and skeletal muscle cells for storage or oxidation, respectively.After removal of the triglyceride core, remnant chylomicron particles are formed. These are high in cholesterol esters and characterized by the presence of apoproteins B, CIII, and E. These remnants are cleared from the circulation by binding of their E apoprotein to a receptor present only on the surface of hepatic cells. Subsequently, the bound remnants are taken to the inside of hepatic cells by endocytosis and then catabolized by lysosomes. This process liberates cholesterol, which is then either converted into bile acids, excreted in bile, or incorporated into lipoproteins originated in the liver (VLDL).
Under normal physiologic conditions, chylomicrons are present in plasma for 1 to 5 hours after a meal and may give it a milky appearance. They are usually cleared from the circulation after a 12-hour fast.
Endogenous Pathway
The liver constantly synthesizes triglycerides by utilizing as substrates free fatty acids and carbohydrates; these endogenous triglycerides are secreted into the circulation in the core of very-low-density lipoprotein particles (VLDL). The synthesis and secretion of VLDL at cellular level occur in a process similar to that of chylomicrons, except that a different B apoprotein (B-100 instead of B-48) together with apoproteins C and E intervene in their secretion. Subsequent interaction of the VLDL particles with lipoprotein lipase in tissue capillaries leads to hydrolysis of the core triglycerides and production of smaller remnant VLDL particles rich in cholesterol esters (intermediate-density lipoproteins, IDL) and liberation of free fatty acids. Around half of these remnant particles are removed from the circulation in 2 to 6 hours as they bind tightly to hepatic cells. The rest undergo modifications with detachment of the remaining triglycerides and its substitution by cholesterol esters and removal of all the apoproteins except apoprotein B. This process results in transformation of the remnant VLDL particles into low-density lipoprotein particles (LDL) rich in cholesterol. In fact, these last particles contain around three-fourths of the total cholesterol in human plasma, although they constitute only some 7% of the total cholesterol pool. Their predominant function is to supply cholesterol to cells with LDL receptors, like those in the adrenal glands, skeletal muscle, lymphocytes, gonads, and kidneys. The quantity of cholesterol freed from LDL is said to control cholesterol metabolism in the cell through the following mechanisms: (1) increased LDL cholesterol in the cell decreases synthesis of the enzyme 3-hydroxy-3 methylglutaryl coenzyme A (HMG-CoA) reductase, which modulates the intracellular synthesis of cholesterol; (2) increased LDL cholesterol may enhance the storage of cholesterol within the cell by activation of another enzyme; and (3) increased cholesterol within the cell diminishes the synthesis of LDL receptors through a negative feedback process.Besides the above described route for LDL degradation in extrahepatic sites, a so-called scavenger cell pathway has been described. This consists of cells in the reticuloendothelial system which, by phagocytosis, dispose of the excess concentrations of this lipoprotein in plasma.
Transport of High-Density Lipoprotein Cholesterol
High-density lipoproteins are a heterogeneous group of macromolecules with different physical properties and chemical components; two subclasses of HDL have been identified (HDL2 and HDL3) within which several subspecies have also been demonstrated. The predomination function of HDL seems to be the reverse transport of cholesterol from different tissues into the liver, where it is eventually removed. Subclass HDL2 has been reported to have a better correlation with coronary artery disease protection than total HDL cholesterol.The serum concentration of HDL and its components derives from various complex intravascular and cellular metabolic events. These events include secretion of precursor HDL particles from the liver and small intestine, interaction of these particles with lipids and proteins released during the catabolism of triglyceride-rich lipoproteins, and production of cholesteryl esters (the core substance in HDL) from the action of lecithin–cholesterol acyltransferase (LCAT), an enzyme that originates in the liver. This enzyme acts on unesterified cholesterol released into plasma from cellular turnover. The cholesterol esters formed in this reaction are in turn transferred to VLDL and subsequently appear in LDL. The end result is a system that allows the transfer of cholesterol through LDL to peripheral cells and its return to the liver through HDL, and that prevents excessive accumulation of cholesterol in the body.
Clinical Significance
Cholesterol and triglycerides, like many other essential components of the body, attract clinical attention when present in abnormal concentrations. Increased or decreased levels usually occur because of abnormalities in the synthesis, degradation, and transport of their associated lipoprotein particles. When hyperlipidemia or hypolipidemia are defined in terms of the class or classes of increased or decreased plasma lipoproteins, the names hyperlipoproteinemia or hypolipoproteinemia are preferentially employed.Hyperlipoproteinemia is the lipid disturbance of major relevance clinically because of its association with an increased risk of atherosclerotic cardiovascular disease. Multiple epidemiologic studies have demonstrated that increased levels of plasma total cholesterol and low-density lipoproteins are strongly and directly related to a greater incidence of coronary heart disease. Elevated plasma triglycerides and very-low-density lipoproteins are directly associated with the risk of atherosclerotic heart disease, although not as independent risk factors. In contrast, high levels of high-density lipoprotein cholesterol have been found to be a protective factor for the development of that disease, so that decreased levels constitute a risk factor.
Clinical manifestations of hyperlipoproteinemia include a greater incidence of ischemic vascular disease, acute pancreatitis, and visible accumulations of lipid deposits (xanthomas and xanthelasmas). The localization of these lesions is of great help in many instances to categorize the lipoprotein dysfunction present.
Increased concentration of plasma lipids is etiologically related mainly to genetic disorders, dietary factors (such as ingestion of excessive calories, saturated fatty acids and cholesterol), or ingestion of drugs, or it may occur as a secondary phenomenon in a large variety of diseases. In any of these instances the elevation of the different plasma lipoproteins usually occurs in a number of combinations that have led to their classification into six different patterns or phenotypes (Table 31.3). Genetic or acquired disorders may be related to one or more of these lipoprotein patterns, so the identification of a particular pattern gives no specific information regarding the cause of the hyperlipidemic disorder in question. A practical approach is to classify the different hyperlipidemic: states into those that mainly cause hypercholesterolemia (Table 31.4) or those that predominantly cause hypertriglyceridemia (Table 31.5). In each of these categories primary (genetic) as well as secondary disorders are included. The genetic disorders in turn could result from a single gene disturbance either of dominant or recessive inheritance, or a polygenic derangement in which multiple genes interact with environmental factors. The main characteristics of primary hyperlipoproteinemias are included in Table 31.6.
For the diagnosis of the different lipoprotein disorders, one can usually rely on simple plasma values of total cholesterol and triglycerides. These measurements should be repeated at least once, so as to obtain a more reliable estimate of the patient's level. Obtained lipid values should be interpreted in relation to age and sex according to reference values established by the Lipid Research Clinics Program (Tables 31.7, 31.8, and 31.9). As stated previously, the diagnosis of hyperlipidemia is based on arbitrary reference values above the 95th percentile for the distribution of cholesterol, triglyceride or LDL cholesterol for a given population. Low reference values (5th percentile for the distribution of cholesterol, LDL and HDL) identify persons with low lipid levels.
Plasma cholesterol and triglyceride values provide information concerning the lipoprotein particles that are increased. Plasma cholesterol values represent total cholesterol, which includes both unesterified cholesterol and cholesteryl esters. Isolated elevation of plasma cholesterol usually indicates that LDL is increased. Isolated elevation of plasma triglyceride points to an elevation in chylomicrons, VLDL, and/or remnants.
The bedside inspection of a refrigerated fasting plasma sample, the measurement of HDL cholesterol (advisable if total plasma cholesterol is persistently elevated) and the evaluation of associated clinical findings provide useful information. In all cases, a detailed history and physical examination is imperative. Evaluation and exclusion of secondary disorders, if necessary, could require additional laboratory tests as indicated in each particular case. Screening of first-degree relatives is advisable, especially if no secondary disorder is evident, as it may reveal a genetic problem. Only in selected instances will special tests or lipoprotein electrophoresis be required for exact genotypic diagnosis.
Hypercholesterolemia
Three primary disorders causing hypercholesterolemia have been identified. They are: (1) polygenic hypercholesterolemia, (2) familial hypercholesterolemia, and (3) a variant of familial combined hyperlipidemia.Polygenic hypercholesterolemia is the term utilized to describe the most common primary disorder causing an increase in plasma cholesterol. It includes a group of related disorders in which multiple genes apparently interact to cause an elevation in LDL above the 95th percentile in the general population. Increased rate of formation of LDL, defective clearance of LDL, or both could be responsible for this elevation. Recent evidence suggests that this may result from a reduced activity of hepatic LDL receptors. Clinical distinction between this disorder and familial hypercholesterolemia and familial combined hyperlipidemia is mainly obtained by family studies and examination for tendon xanthomas. Hyperlipidemia occurs in only 10% of the first-degree relatives in the polygenic disorder, while it occurs in around 50% of the relatives in the other two conditions. Tendon xanthomas are not found in both the polygenic disorder and familial combined hyperlipidemia but occur in around 75% of adult heterozygotes with familial hypercholesterolemia. Epidemiologic studies indicate that subjects with this disorder are at particularly high risk for coronary artery disease.
Familial hypercholesterolemia is a common autosomal dominant disorder that affects approximately 1:500 persons in the general population. Its principal defect lies in the gene for the LDL receptor on the surface of cells so that clearance of LDL from plasma is delayed. Homozygotes are rare and usually attain a six- to eightfold increase in total plasma cholesterol due to an elevation in LDL; heterozygotes may have a two- to threefold elevation and can be diagnosed at birth with analysis of umbilical cord blood. The most important clinical characteristic of this disorder is the presence of premature and accelerated coronary artery disease. Heterozygotes manifest myocardial infarctions around the third decade, while homozygotes usually die of myocardial infarction complications before age 20. The second most important finding is the presence of xanthomas over tendons. Although tendon xanthomas are virtually diagnostic of the condition, their absence does not exclude it. Other associated findings include xanthelasmas and arcus corneae.
Familial hypercholesterolemia can be diagnosed in sophisticated laboratories by direct measurement of the number of LDL receptors on freshly isolated lymphocytes or on cultured skin fibroblasts. It has been diagnosed in utero by the absence of LDL receptors on cultured amniotic fluid cells.
Familial combined hyperlipidemia is another common disorder that has an autosomal dominant inheritance. It can present clinically as hypercholesterolemia (type 2a), hypertriglyceridemia (type 4) or both (type 2b) and has also been called multiple-type hyperlipoproteinemia. It is characterized clinically by the absence of hyperlipoproteinemia during childhood, and its development occurs around puberty in association with variable and mild elevation in plasma lipid levels. There is no specific clinical or laboratory test to determine if an individual has this disorder, and family screening is needed in order to make the diagnosis. Nevertheless, it should be suspected in any individual with a mild hyperlipoproteinemia whose lipoprotein type changes with time. This condition is also characterized by an increased incidence of premature atherosclerosis and myocardial infarction. The basic abnormality apparently is overproduction of lipoproteins that contain apolipoprotein B (apo B).
Various common disorders are associated with hypercholesterolemia. Among these are hypothyroidism, nephrotic syndrome, dysproteinemias, obstructive liver disease, and use of thiazide diuretics.
Hypertriglyceridemia
The primary disorders predominantly causing hypertriglyceridemia are: (1) familial hypertriglyceridemia, (2) familial combined hyperlipidemia, (3) congenital deficiency of lipoprotein lipase, (4) deficiency of apoprotein CII and (5) familial dysbetalipoproteinemias.Familial hypertriglyceridemia is a common autosomal dominant disorder characterized by increased plasma concentration of VLDL (type 4 lipoprotein pattern). Moderate elevations of triglycerides usually occur during early adulthood, and a triad of obesity, hyperglycemia, and hyperinsulinemia can be seen in affected individuals. In individuals with moderate elevation in plasma triglycerides associated with a normal cholesterol level, the possibility of familial hypertriglyceridemia should be suspected.
Although patients with this disorder usually have moderate elevation of plasma triglycerides, whenever conditions known to elevate this lipid fraction, such as diabetes mellitus or alcohol or oral contraceptive consumption, concurrently occur, they may develop a profound hypertriglyceridemia and a mixed hyperlipidemia (type 5 lipoprotein pattern). An increased incidence of atherosclerosis has been reported. Hypertension and hyperuricemia have also been frequently observed.
Familial combined hyperlipidemia has already been discussed under Hypercholesterolemia.
Congenital lipoprotein lipase deficiency is a rare autosomal recessive disorder secondary to absence or severe diminution in the activity of lipoprotein lipase. Affected individuals are homozygous for a mutation that prevents normal expression of lipoprotein lipase activity. The parents, although clinically normal, are obligate heterozygotes. This enzymatic disorder is reflected in a massive accumulation of chylomicrons in the plasma without elevation of VLDL (type 1 lipoprotein pattern). Triglycerides may reach levels of 2000 to 10,000 mg/dl. This disorder usually appears in childhood with recurrent bouts of abdominal pain secondary to pancreatitis. Another characteristic feature of the disorder is the occurrence of eruptive xanthomas, predominantly in the buttocks and other pressure-sensitive areas of the body, attributed to the deposition of chylomicron triglycerides in histiocytes. The elevation in chylomicrons may also cause a lipemic serum, a picture of lipemia retinalis, and hepatosplenomegaly. The diagnosis is suspected by the presence of a lipemic plasma in a young patient who has fasted for 12 hours. Overnight incubation of a test tube of such plasma in a refrigeration at 4°C demonstrates a visible white layer at the top of the tube. Failure of lipoprotein lipase levels to increase after an infusion of heparin confirms the diagnosis. The occurrence of accelerated atherosclerosis is not reported in this condition.
Apoprotein CII deficiency is a rare autosomal recessive disorder caused by absence of apoprotein CII, a required co-factor for the activity of lipoprotein lipase. The ensuing functional deficiency in this enzyme leads to a clinical picture similar to that described above for congenital lipoprotein lipase deficiency. However, in contrast to what occurs in the latter disorder, affected individuals are diagnosed at later age and rarely present eruptive xanthomas. The usual presentation is also with recurrent abdominal pains secondary to acute pancreatitis. At times the diagnosis is made by chance discovery of a milky serum.
Due to the inherent defect in this condition, in which lipoprotein lipase is not activated, both chylomicrons and VLDL are elevated in the blood causing a type 1 or type 5 lipoprotein pattern.
Familial dysbetalipoproteinemia, also called familial type 3 hyperlipoproteinemia, is a condition inherited through a single gene mechanism whose clinical presentation requires the presence of other genetic or environmental factors. Elevation of both plasma cholesterol and triglycerides occurs because of accumulation of remnant VLDL particles in the plasma. The metabolic defect in most patients occurs in apolipoprotein E. This has three common alleles, designated E2, E3, and E4. Patients with this disorder have only apolipoprotein E2 in VLDL, which is less effective in facilitating clearance of remnants than E3 or E4. The condition occurs only in individuals who are homozygous for E2, that is, those with an E2/E2 genotype. Clinical evidence of hyperlipoproteinemia usually appears after the second decade. The characteristic clinical findings are xanthoma striata palmaris and tuberous and tuberoeruptive xanthomas over the elbows and knees. The disorder is associated with severe atherosclerosis of the coronary arteries, abdominal aorta, and peripheral arteries.
The diagnosis is facilitated by encountering a broad beta band on lipoprotein electrophoresis. Confirmation can be obtained in specialized laboratories either by measuring the chemical composition of the VLDL fraction after ultracentrifugation of the plasma or by determining for the E2 allele after isoelectric focusing of remnant proteins.
Table 31.10Percentiles for Plasma Total High-Density Lipoprotein Cholesterol (mg/dl) in the Normal White North American Population
| Men | Women | ||||
|---|---|---|---|---|---|
| Age (yr) | 5 | 95 | Age (yr) | 5 | 95 |
| 5–14 | 35 | 75 | 5–19 | 35 | 70 |
| 15–19 | 30 | 65 | 20–24 | 35 | 80 |
| 20–24 | 30 | 65 | 25–34 | 35 | 80 |
| 25–29 | 30 | 65 | 35–39 | 35 | 80 |
| 30–34 | 30 | 65 | 40–44 | 35 | 90 |
| 35–39 | 30 | 60 | 45–49 | 35 | 85 |
| 40–44 | 25 | 65 | 50–54 | 35 | 90 |
| 45–69 | 30 | 70 | 55 + | 35 | 95 |
| 70 + | 30 | 75 | |||
- Source: Abridged from Lipid Research Clinic Data, 1983.
Hyperalphalipoproteinemia
Another clinical condition associated with elevation in plasma lipoproteins is hyperalphalipoproteinemia, characterized by elevated plasma levels of high-density lipoproteins. The elevation in HDL leads to slight increase in total plasm cholesterol values. Other plasma lipid components (LDL, VLDL, and triglycerides) are normal.The majority of cases of hyperalphalipoproteinemia are genetic with either a dominant or polygenic inheritance. Secondary elevations of HDL have been related to various factors such as weight reduction, regular exercise, moderate alcohol intake, estrogen administration, exposure to chlorinated hydrocarbon pesticides, and biliary cirrhosis. Patients with this condition usually do not present any distinguishing clinical features. As previously mentioned, hyperalphalipoproteinemia is associated with a decreased risk of coronary atherosclerosis and with increased longevity.
Hypolipoproteinemias
Hypoalphalipoproteinemia probably is the most clinically significant hypolipoproteinemia in view of the fact that considerable evidence suggests that low levels of plasma HDL cholesterol are related to an increased incidence of coronary heart disease in high-risk populations.According to the NIH Consensus Conference, the finding of HDL cholesterol values below 35 mg/dl constitutes an independent risk factor for coronary artery disease. Several factors have been identified as causing a decrease in HDL cholesterol. These include ill-defined genetic factors, obesity, cigarette smoking, physical inactivity, hypertriglyceridemia, oral contraceptives, beta-adrenergic blocking drugs, thiazide diuretics, and cholesterol-reducing diets.
Other hypolipoproteinemias comprise two rare disorders characterized by a decrease in the concentration of lipids in plasma and an autosomal recessive inheritance.
Abetalipoproteinernia usually appears early in childhood, and because of a defective production of apoprotein B, there is absence of chylomicrons, VLDL, and LDL in the plasma. The plasma cholesterol level is usually less than 75 mg/dl and that of triglycerides less than 15 mg/dl. The main clinical features are malabsorption of fats, peripheral neuropathy, ataxia, retinitis pigmentosa, and acanthocytosis.
Tangier disease is a condition that also manifests in childhood and is characterized by the absence of HDL from the plasma. This defect leads to the production of abnormal chylomicron remnants, which are stored as cholesterol esters in cells of the phagocytic system. Levels of plasma cholesterol are usually less than 100 mg/dl and that of triglycerides range from 100 to 250 mg/dl. The main clinical features are enlarged orange tonsils, corneal opacities, and infiltration of the bone marrow and the intestinal mucosa. Patients with this illness are at increased risk for premature atherosclerosis.
Dyslipoproteinemia, is the term utilized for conditions in which structurally abnormal lipoproteins circulate in plasma. Such a defect is seen in lecithin cholesterol acyltransferase (LCAT) deficiency. This is a rare disorder in which decreased activity of this enzyme leads to a large accumulation of unesterified cholesterol in plasma and body tissues. Laboratory findings include a variable level of total plasma cholesterol with decreased esterified cholesterol, an increase in unesterified cholesterol and increased VLDL. The structure of all the lipoproteins is abnormal. The condition usually presents in young adulthood with corneal opacities, renal insufficiency, hemolytic anemia, and premature atherosclerosis.
References
- Ad Hoc Committee of AHA to Design a Dietary Treatment of Hyperlipoproteinemia. Recommendations for Treatment of Hyperlipidemia in Adults. A Joint Statement of the Nutrition Committee and the Council on Arteriosclerosis. Circulation. 1984;72:1067A–90A.
- Brewer HB, Zech LA, Greg , RE, Schwartz D, Schaefer EJ. Type III hyperlipoproteinemia: diagnosis, molecular defects, pathology, and treatment. Ann Intern Med. 1983;98:623–40. [PubMed: 6846977]
- Brown MS, Goldstein JS. How LDL receptors influence cholesterol and atherosclerosis. Sci Am. 1984;251:57–66. [PubMed: 6390676]
- Castelli WP, Cooper GR, Doyle JT, Garcia-Palmieri MR, Gordon T, Homes C, Hudley SB, Kagan A, Kuckmak M, McGee D, Vicic WJ. Distribution of triglyceride and total LDL and HDL cholesterol in several populations: a cooperative lipoprotein phenotyping study. J Chron Dis. 1977;30:147–69. [PubMed: 191465]
- Council on Scientific Affairs, Division of Scientific Analysis and Technology, American Medical Association. Dietary and pharmacology therapy for the lipid risk factors. JAMA. 1983;250:1873–79. [PubMed: 6620484]
- Goldstein JL, Kita T, Brown MS. Defective lipoprotein receptors and atherosclerosis. N Engl J Med. 1983;309:288–96. [PubMed: 6306464]
- Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease. Am J Med. 1977;62:707–14. [PubMed: 193398]
- Havel RJ. Approach to the patient with hyperlipidemia. Med Clin N Amer. 1982;66:319–33. [PubMed: 7070147]
- Hulley SB, Lo B. Choice and use of blood lipid tests. Arch Intern Med. 1984;143:667–73. [PubMed: 6340621]
- Lipid Research Clinics Program. Lipid and lipoprotein analysis. Vol. 1, in Manual of laboratory operations. NIH publication 75–628. Bethesda, Md.: U.S. Department of Health and Human Services, 1974 (revised October 1982).
- Naito H. Reliability of lipid and lipoprotein testing 1. Am J Cardiol. 1985;56:9 J.
- National Institutes of Health Consensus Conference. Lowering blood cholesterol to prevent heart disease. JAMA. 1985;253:2080. [PubMed: 3974099]
- Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. The Expert Panel. Arch Intern Med. 1988;148:36–69. [PubMed: 3422148]
- Rifkind BM, Segal P. Lipid Research Clinics Program reference values for hyperlipidemia and hypolipidemia. JAMA. 1983;250:1869–72. [PubMed: 6578354]
- Stanbury JB, et al, eds. The metabolic basis of inherited disease, 5th ed. New York: McGraw-Hill, 1983, Chaps. 29, 31, 34.
Figures
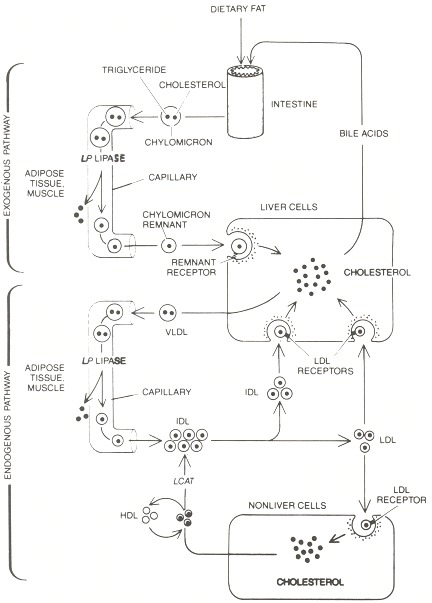
Figure 31.1
Exogenous and endogenous fat-transport pathways are diagrammed. Dietary cholesterol is absorbed through the wall of the intestine and is packaged, along with triglyceride (glycerol ester-linked to three fatty acid chains), in chylomicrons. In the capillaries of fat and muscle tissue the triglyceride's ester bond is cleaved by the enzyme lipoprotein (LP) lipase and the fatty acids are removed. When the cholesterol-rich remnants reach the liver, they bind to specialized receptors and are taken into liver cells. Their cholesterol either is secreted into the intestine (mostly as bile acids) or is packaged with triglyceride in very-low-density lipoprotein (VLDL) particles and secreted into the circulation, inaugurating the endogenous pathway. Again the triglyceride is removed in fat or muscle, leaving cholesterol-rich intermediate-density lipoprotein (IDL). Some IDL binds to liver LDL receptors and is rapidly taken up by liver cells; the remainder stays in the circulation and is converted into LDL. Most of the LDL binds to LDL receptors on liver or other cells and is removed from the circulation. Cholesterol leaching from cells binds to high-density lipoprotein (HDL) and is esterified by the enzyme LCAT. The esters are transferred to IDL and then LDL and are eventually taken up again by cells. From Brown MS, Goldstein JS. How HDL receptors influence cholesterol and atherosclerosis. Copyright © 1984 by Scientific American, Inc. All rights reserved.
Tables
Table 31.1Lipoproteins Present on Electrophoresis
| Electrophoretic fraction | Finding on ultracentrifugation |
|---|---|
| Nonmigrating band | Chylomicrons |
| Beta band | LDL |
| Broad beta band | IDL |
| Pre-beta band | VLDL |
| Alpha band | HDL |
Table 31.2Characteristics and Percentage Content of the Various Lipoprotein Particles Relative to Total Weight
| Lipoprotein particle | Size (Å) | Density | Mobility by electrophoresis | Cholesterol percentage | Triglyceride percentage | Phospholipid percentage | Apoprotein percentage | Major apoproteins |
|---|---|---|---|---|---|---|---|---|
| Chylomicrons | 800–5000 | 0.95 | Remains at origin | 3 | 90 | 5 | 9 | AI. AII, B, CI. CII, CIII |
| Very-low-density lipoprotein (VLDL) | 300–800 | 0.95–1.006 | Pre-beta | 10 | 70 | 10 | 10 | BI, CI, CII, CIII, E |
| Intermediate-density lipoprotein (IDL) | 250–350 | 1.006–1.019 | Slow pre-beta | – | – | – | – | B, CIII, E |
| Low-density lipoprotein (LDL) | 180–280 | 1.019–1.063 | Beta | 26 | 10 | 15 | 25 | B |
| High-density lipoprotein (HDL) | 50–120 | 1.063–1.210 | Alpha | 20 | 5 | 25 | 50 | AI, All |
Table 31.3Lipoprotein Patterns Resulting from Elevation of Different Plasma Lipid Fractions
| Lipoprotein pattern | Increased lipid fraction | Predominant lipoprotein |
|---|---|---|
| Type I | Triglycerides | Chylormicrons |
| Type 2a | Cholesterol | LDL |
| Type 2b | Cholesterol and triglycerides | LDL and VLDL |
| Type 3 | Triglycerides and cholesterol | Remnants |
| Type 4 | Triglycerides | VLDL |
| Type 5 | Triglycerides and cholesterol | VLDL and chylomicrons |
Table 31.4Disorders Mainly Causing Hypercholesterolemia
| Primary disorders |
 Polygenic hypercholesterolemia Polygenic hypercholesterolemia |
 Familial hypercholesterolemia Familial hypercholesterolemia |
 Familial combined hyperlipidemia Familial combined hyperlipidemia |
| Secondary disorders |
 Hyperthyroidism Hyperthyroidism |
 Nephrotic syndrome Nephrotic syndrome |
 Dysproteinemias Dysproteinemias |
 Obstructive liver disease Obstructive liver disease |
 Thiazide diuretics Thiazide diuretics |
Table 31.5Disorders Mainly Causing Hypertriglyceridemia
| Primary disorders |
 Familial hypertriglyceridemia Familial hypertriglyceridemia |
 Familial combined hyperlipidemia Familial combined hyperlipidemia |
 Congenital deficiency of lipoprotein lipase Congenital deficiency of lipoprotein lipase |
 Deficiency of apoprotein CII Deficiency of apoprotein CII |
 Familial dysbetalipoproteinemia Familial dysbetalipoproteinemia |
| Secondary disorders |
 Uncontrolled diabetes mellitus Uncontrolled diabetes mellitus |
 Nephrotic syndrome Nephrotic syndrome |
 Dysproteinemias Dysproteinemias |
 Oral contraceptives Oral contraceptives |
 Thiazide diuretics Thiazide diuretics |
 Beta-adrenergic blocking agents Beta-adrenergic blocking agents |
 Alcohol Alcohol |
Table 31.6Characteristics of Primary Hyperlipoproteinemias
| Condition | Hereditary pattern | Frequency | Biochemical defect | Plasma lipids | Elevated lipoprotein | Lipoprotein pattern | Major clinical features |
|---|---|---|---|---|---|---|---|
| Polygenic hypercholesterolemia | Multiple genes | Very common | Reduced activity hepatic LDL receptor | Increased cholesterol; TG normal | LDL | 2a | Adult onset; accelerated atherosclerosis |
| Familial hypercholesterolemia | Autosomal dominant | Common 1:500 | Deficiency of LDL receptor | Increased cholesterol; TG normal | LDL | 2a (rarely 2b) | Onset at all ages; planar, tendinous, tuberous xanthomas; accelerated atherosclerosis |
| Familial combined hyperlipidemia | Autosomal dominant | Common | Unknown | Increased cholesterol; TG normal | LDL and VLDL | Onset at all ages; accelerated atherosclerosis | |
| Familial hypertriglyceridemia | Autosomal dominant | Common | Unknown | Cholesterol normal; TG greatly increased | VLDL (rarely chylomicrons) | 4 (rarely 5) | Adult onset; eruptive xanthomas may occur; accelerated atherosclerosis; hyperglycemia; hyperuricemia; hepatosplenomegaly |
| Congenital lipoprotein lipase deficiency | Autosomal recessive | Rare | Deficiency of lipoprotein lipase | Normal cholesterol ; TG greatly increased | Chylomicrons | 1 | Juvenile onset; eruptive xanthomas; pancreatitis; lipemic plasma; lipemia retinalis; hepatosplenomegaly |
| Deficiency of apoprotein CII | Autosomal recessive | Rare | Deficiency of apoprotein CII | Normal cholesterol; TG greatly increased | Chylomicrons and VLDL | 1 or 5 | Juvenile onset; pancreatitis; lipemic plasma |
| Familial dysbetalipoproteinemia | Single mutant gene | Rare | Abnormal apoprotein E of VLDL | Increased cholesterol; TG increased | Remnants | 3 | Adult onset; palmar and/or tubereruptive xanthomas; accelerated atherosclerosis |
Table 31.7Percentiles for Plasma Total Cholesterol (mg/dl) in the Normal White North American Population
| Men | Women | ||||||
|---|---|---|---|---|---|---|---|
| Age (yr) | 5 | 75 | 95 | Age (yr) | 5 | 75 | 95 |
| 0–19 | 115 | 175 | 200 | 0–19 | 120 | 175 | 200 |
| 20–24 | 125 | 185 | 220 | 20–24 | 125 | 190 | 230 |
| 25–29 | 135 | 200 | 245 | 25–34 | 130 | 195 | 235 |
| 30–34 | 140 | 215 | 255 | 35–39 | 140 | 205 | 245 |
| 35–39 | 145 | 225 | 270 | 40–44 | 145 | 215 | 255 |
| 40–44 | 150 | 230 | 270 | 45–49 | 150 | 225 | 270 |
| 45–69 | 160 | 235 | 275 | 50–54 | 165 | 240 | 285 |
| 70 + | 150 | 230 | 270 | 55 + | 170 | 250 | 295 |
- Source: Abridged from Lipid Research Clinic Data, 1983.
Table 31.8Percentiles for Plasma Triglycerides (mg/dl) in the Normal White North American Population
| Men | Women | ||||
|---|---|---|---|---|---|
| Age (yr) | 5 | 95 | Age (yr) | 5 | 95 |
| 0–9 | 30 | 100 | 0–9 | 35 | 110 |
| 10–14 | 30 | 125 | 10–19 | 40 | 130 |
| 15–19 | 35 | 150 | 20–34 | 40 | 170 |
| 20–24 | 45 | 200 | 35–39 | 40 | 195 |
| 25–29 | 45 | 250 | 40–44 | 45 | 210 |
| 30–34 | 50 | 265 | 45–49 | 45 | 230 |
| 35–39 | 55 | 320 | 50–54 | 55 | 240 |
| 40–54 | 55 | 320 | 55–64 | 55 | 250 |
| 55–64 | 60 | 290 | 65 + | 60 | 240 |
| 65 + | 55 | 260 | |||
- Source: Abridged from Lipid Research Clinic Data, 1983.
Table 31.9Percentiles for Plasma Total Low-Density Lipoprotein Cholesterol (mg/dl) in the Normal White North American Population
| Men | Women | ||||||
|---|---|---|---|---|---|---|---|
| Age (yr) | 5 | 75 | 95 | Age (yr) | 5 | 75 | 95 |
| 0–19 | 65 | 105 | 130 | 0–19 | 65 | 110 | 140 |
| 20–24 | 65 | 120 | 145 | 20–24 | 55 | 120 | 160 |
| 25–29 | 70 | 140 | 165 | 25–34 | 70 | 125 | 160 |
| 30–34 | 80 | 145 | 185 | 35–39 | 75 | 140 | 170 |
| 35–39 | 80 | 155 | 190 | 40–44 | 75 | 145 | 175 |
| 40–44 | 85 | 155 | 185 | 45–49 | 80 | 150 | 185 |
| 45–69 | 90 | 165 | 205 | 50–54 | 90 | 160 | 200 |
| 70 + | 90 | 165 | 185 | 55 + | 95 | 170 | 215 |
- Source: Abridged from Lipid Research Clinic Data. 1983.
Copyright © 1990, Butterworth Publishers, a division of Reed Publishing.
It is the intent to provide valuable information and best practices, including an understanding of the regulatory process.
Trả lờiXóafoods to avoid with hyperthyroidism