The physician cannot prescribe by letter, he must feel the pulse.
—seneca
The arterial pulse is the abrupt expansion of an artery resulting from the sudden ejection of blood into the aorta and its transmission throughout the arterial system. The impulse that results from left ventricular ejection can be transmitted down the aorta at a velocity 20 times greater than the velocity of the ejected blood bolus. The peak of this arterial pulse is the systolic blood pressure.
Pulses should be palpated when the patient is in a reclining or resting position. The index finger or thumb can lightly compress the artery during auscultation of the heart. The heart sounds can then be used as reference points for systole and diastole. An attempt to create a mental image of the arterial pulse, its ascending limb, peak, and descending limb, enhances the value of palpation. Practice this in the intensive care unit (ICU) where a patient may have a radial artery line measuring pressure on an oscilloscope. Palpation of the opposite radial artery while observing the pulse contour on the scope can enhance palpation skills. Deep palpation may be necessary for subclavian, popliteal, or femoral pulses, particularly in obese patients. Flexing the knee and holding it while palpating the popliteal space perpendicular to the artery helps in examination of the popliteal artery.
The arterial pulse changes as it travels from the central aorta down to the peripheral arteries. Although mean blood pressure decreases from the central aorta to the peripheral arteries, the systolic pressure increases. The pulse can be distorted and damped by reflected, resonance, or standing waves, as well as differences in the elastic properties and caliber of the peripheral arteries of the upper and lower parts of the body. The size of the normal arterial pulse is affected by the left ventricular ejection volume and the rate of ejection, as well as the elasticity or distensibility of the peripheral arteries. The greater the distance from the heart to a peripheral artery, the greater will be the distortion of the arterial pulse peripherally. Because complex factors affect the contour of the arterial pulse as it is transmitted through the arterial system, careful examination of the most central arterial pulse, the carotid, is necessary for pulse contour information.
Although the carotid pulse is important, there is much to be learned from an examination of all pulses bilaterally: subclavian, brachial, femoral, popliteal, posterior tibial, and dorsalis pedis. Palpation of the peripheral arteries can be performed whenever they are close enough to the skin surface to be compressed. Auscultation of these arteries, especially the carotid, subclavian, and femoral, can reveal bruits suggesting partial obstruction. The pulse rate, rhythm, and quality can be examined. In addition, the patency and pliability of the artery can be assessed.
Although the carotid pulse is important, there is much to be learned from an examination of all pulses bilaterally: subclavian, brachial, femoral, popliteal, posterior tibial, and dorsalis pedis. Palpation of the peripheral arteries can be performed whenever they are close enough to the skin surface to be compressed. Auscultation of these arteries, especially the carotid, subclavian, and femoral, can reveal bruits suggesting partial obstruction. The pulse rate, rhythm, and quality can be examined. In addition, the patency and pliability of the artery can be assessed.
Because peripheral pulse contour is determined by left ventricular ejection and vascular properties, emphasis is placed on the presence or absence of a pulse, and on hypokinetic or hyperkinetic pulses. Absence of a pulse could suggest occlusion by thrombus, embolus, or dissection. Absence or diminished leg pulses may confirm a vascular etiology of intermittent claudication.
If the pulse is present but of low volume and amplitude, it is hypokinetic. This could suggest low cardiac output in shock or myocardial infarction. Idiopathic dilated cardiomyopathy, valvular stenosis, pericardial tamponade, or constrictive pericarditis can also cause low cardiac output and small peripheral pulses.
Severe aortic stenosis causes a small pulse known as pulsus parous et tardus. It is a low-amplitude pulse with a delayed upstroke (Figure 17.1). This is best palpated on the carotid artery.
 In contrast to low-amplitude arterial pulses are those large-amplitude and strong pulses that are normal. If these become bounding, they are called hyperkinetic. Anxiety, exercise, fever, hyperthyroidism, and anemia can cause a hyperkinetic pulse in a normal person with a large left ventricular stroke volume and an otherwise normal cardiovascular system.
In contrast to low-amplitude arterial pulses are those large-amplitude and strong pulses that are normal. If these become bounding, they are called hyperkinetic. Anxiety, exercise, fever, hyperthyroidism, and anemia can cause a hyperkinetic pulse in a normal person with a large left ventricular stroke volume and an otherwise normal cardiovascular system.
Hyperkinetic pulses can also occur where there is a rapid peripheral runoff of blood in addition to a large stroke volume from the left ventricle. Patent ductus arteriosus with normal pulmonary pressures, large arterial venous fistulas, and severe aortic regurgitation can cause these hyperkinetic pulses. The pulse of severe aortic regurgitation is described as water-hammer and collapsing. Severe aortic regurgitation can also cause a pulse in the fingernail bed (Quincke's pulse), best demonstrated by placing a penlight on the fingerpad and casting light through the fingernail from behind. Varying the pressure of the penlight on the fingerpad will bring out the Quincke's pulse. Some of these patients will have a double systolic pulse called a bisferiens pulse. This occurs when some aortic stenosis accompanies the severe aortic regurgitation. These two waves are called the percussion wave followed by a tidal wave—both in systole (Figure 17.2). The bisferiens pulse is strongly associated with idiopathic hypertrophic subaortic stenosis.
 In addition to twice-beating systolic pulses, the bisferiens, there are twice-beating or bifid pulses where one impulse occurs in systole and one occurs in diastole. These can be seen when the peripheral resistance or the diastolic blood pressure is low. Low cardiac output states can allow the systolic and diastolic pulses to become nearly equal and potentially palpable (see Figures 17.4 and 17.5).
In addition to twice-beating systolic pulses, the bisferiens, there are twice-beating or bifid pulses where one impulse occurs in systole and one occurs in diastole. These can be seen when the peripheral resistance or the diastolic blood pressure is low. Low cardiac output states can allow the systolic and diastolic pulses to become nearly equal and potentially palpable (see Figures 17.4 and 17.5).
 A common cause of a double-beating pulse is intra-aortic balloon counterpulsation (Figure 17.3). The balloon catheter is placed in the descending aorta below the takeoff of the left subclavian artery and pulses in diastole. The balloon is timed to expand after closure of the aortic valve. The balloon is evacuated and collapses just before left ventricular ejection. In Figure 17.3, note the lower diastolic pressure (D) that the left ventricle faces after a pump pulse. If the pump pulse or diastolic pressure is significantly higher than the systolic pressure generated by the left ventricle, the patient may be hypovolemic.
A common cause of a double-beating pulse is intra-aortic balloon counterpulsation (Figure 17.3). The balloon catheter is placed in the descending aorta below the takeoff of the left subclavian artery and pulses in diastole. The balloon is timed to expand after closure of the aortic valve. The balloon is evacuated and collapses just before left ventricular ejection. In Figure 17.3, note the lower diastolic pressure (D) that the left ventricle faces after a pump pulse. If the pump pulse or diastolic pressure is significantly higher than the systolic pressure generated by the left ventricle, the patient may be hypovolemic.
 Another abnormal pulse is called pulsus alternans. This is a regular pulse with alternation of beat amplitude every other beat. It is associated with severe left ventricular failure of any cause. These amplitude changes will be emphasized in a peripheral artery and may be easiest to detect in the femoral pulse (Figure 17.4).
Another abnormal pulse is called pulsus alternans. This is a regular pulse with alternation of beat amplitude every other beat. It is associated with severe left ventricular failure of any cause. These amplitude changes will be emphasized in a peripheral artery and may be easiest to detect in the femoral pulse (Figure 17.4).
If the pulse decreases dramatically in amplitude with inspiration and increases with expiration, it is called pulsus paradoxus. Actually this is an exaggeration of a normal physiologic phenomenon. On inspiration, there is some pooling of blood in the lungs and a transient decline in venous return to the left ventricle. Therefore, left ventricular stroke volume declines slightly. If the fall in systolic blood pressure is greater than 10 mm Hg, it is abnormal (Figure 17.5). This is commonly associated with pericardial tamponade, but any cause of decreased venous return to the left ventricle can cause pulsus paradoxus. Pericardial tamponade restricts right heart filling, but so does superior vena cava syndrome. In addition, asthma, emphysema, or airway obstruction can cause changes in intrathoracic pressure and effect wide swings in pulmonary blood volume and thus left ventricular venous return. Pulsus paradoxus can result.
Simultaneous palpation of two pulses can be diagnostic. Palpation of the radial and the femoral pulse should yield nearly simultaneous pulses. If there is a palpable delay from the radial to the femoral pulse, it suggests coarctation of the aorta or at least an aortic obstruction below the takeoff of the left subclavian artery. All hypertensive patients should have this examination. Unilateral absence of a pulse can aid in the diagnosis of a dissected aortic aneurysm.
If the carotid pulse is palpated for pulse contour and the femoral pulse for pulses paradoxus, then the radial pulse is palpated for rate and rhythm. The pulse rate and regularity are easily obtained here. The absence of a radial pulse should prompt a search for an ulnar pulse. An irregular pulse can be caused by atrial fibrillation; by premature beats arising in the atria, the atrioventricular junction, or the ventricles; and by second-degree atrioventricular block.
A slow, bounding hyperkinetic pulse can be found in complete heart block. Atrial Fibrillation causes an irregularly, irregular pulse. Not only will the rate of the pulse be irregular, but the pulse amplitude will also vary (Figure 17.6). This results from variable stroke volumes during systole. Note in Figure 17.6 how the systolic pressure varies from beat to beat. If the ventricular rate is rapid, some pulses may not be transmitted to the peripheral circulation. Simultaneous ausculation of the heart and palpation of the radial pulse can allow measurements of an apical to radial pulse deficit. Controlled atrial fibrillation should have no pulse deficit, that is, all central heartbeats are transmitted to the radial pulse and the peripheral circulation.
 Premature beats of any origin can cause irregularities of the pulse. If the premature beats alternate with normal sinus beats, bigeminy results. The results can be a pulse beat that has a strong, large-amplitude pulse (hyperkinetic) alternating with a weak, low-amplitude pulse (hypokinetic) (see Figure 17.7). Irregularities of the pulse rate or rhythm require an electrocardiogram for final diagnosis of the cardiac arrhythmia. Palpation of the pulse is a time-honored part of the physical examination that still contains important information.
Premature beats of any origin can cause irregularities of the pulse. If the premature beats alternate with normal sinus beats, bigeminy results. The results can be a pulse beat that has a strong, large-amplitude pulse (hyperkinetic) alternating with a weak, low-amplitude pulse (hypokinetic) (see Figure 17.7). Irregularities of the pulse rate or rhythm require an electrocardiogram for final diagnosis of the cardiac arrhythmia. Palpation of the pulse is a time-honored part of the physical examination that still contains important information.
If the pulse is present but of low volume and amplitude, it is hypokinetic. This could suggest low cardiac output in shock or myocardial infarction. Idiopathic dilated cardiomyopathy, valvular stenosis, pericardial tamponade, or constrictive pericarditis can also cause low cardiac output and small peripheral pulses.
Severe aortic stenosis causes a small pulse known as pulsus parous et tardus. It is a low-amplitude pulse with a delayed upstroke (Figure 17.1). This is best palpated on the carotid artery.
Figure 17.1
A simultaneous recording of left ventricular and aortic pressures in a patient with severe calcific aortic stenosis. The peak-to-peak pressure gradient is more than 125 mm Hg. Note the anacrotic notch (A) on the delayed upstroke of the aortic pulse.
Hyperkinetic pulses can also occur where there is a rapid peripheral runoff of blood in addition to a large stroke volume from the left ventricle. Patent ductus arteriosus with normal pulmonary pressures, large arterial venous fistulas, and severe aortic regurgitation can cause these hyperkinetic pulses. The pulse of severe aortic regurgitation is described as water-hammer and collapsing. Severe aortic regurgitation can also cause a pulse in the fingernail bed (Quincke's pulse), best demonstrated by placing a penlight on the fingerpad and casting light through the fingernail from behind. Varying the pressure of the penlight on the fingerpad will bring out the Quincke's pulse. Some of these patients will have a double systolic pulse called a bisferiens pulse. This occurs when some aortic stenosis accompanies the severe aortic regurgitation. These two waves are called the percussion wave followed by a tidal wave—both in systole (Figure 17.2). The bisferiens pulse is strongly associated with idiopathic hypertrophic subaortic stenosis.
Figure 17.2
A carotid pulse tracing from a patient with severe aortic regurgitation. Note that the percussion wave (P) is smaller than the tidal wave (T), as it often is. Both percussion and tidal waves occur in systole before the dicrotic notch (DN).
Figure 17.4
This aortic pressure tracing (scale of 0 to 100 mm Hg) was taken from a patient with a severe dilated idiopathic cardiomyopathy. The alternate pressure pulses (A) are 10 mm Hg lower than the pulses preceding them. Pulsus alternans was initiated by a premature (more...)
Figure 17.5
This aortic pressure pulse was recorded (scale of 0 to 200 mm Hg) in a patient with pericardial tamponade. During inspiration (INSP), the peak systolic pressure drops 20 mm Hg. The pulse rate was 120 beats per minute, and the respiratory rate was nearly (more...)
Figure 17.3
Panel A shows the simultaneous recording of the left ventricular and aortic pressures (on a scale of 0 to 200 mm Hg) in a patient with severe coronary artery disease. The aortic pressure is 160/90 mm Hg and the left ventricular end diastolic pressure (more...)
If the pulse decreases dramatically in amplitude with inspiration and increases with expiration, it is called pulsus paradoxus. Actually this is an exaggeration of a normal physiologic phenomenon. On inspiration, there is some pooling of blood in the lungs and a transient decline in venous return to the left ventricle. Therefore, left ventricular stroke volume declines slightly. If the fall in systolic blood pressure is greater than 10 mm Hg, it is abnormal (Figure 17.5). This is commonly associated with pericardial tamponade, but any cause of decreased venous return to the left ventricle can cause pulsus paradoxus. Pericardial tamponade restricts right heart filling, but so does superior vena cava syndrome. In addition, asthma, emphysema, or airway obstruction can cause changes in intrathoracic pressure and effect wide swings in pulmonary blood volume and thus left ventricular venous return. Pulsus paradoxus can result.
Simultaneous palpation of two pulses can be diagnostic. Palpation of the radial and the femoral pulse should yield nearly simultaneous pulses. If there is a palpable delay from the radial to the femoral pulse, it suggests coarctation of the aorta or at least an aortic obstruction below the takeoff of the left subclavian artery. All hypertensive patients should have this examination. Unilateral absence of a pulse can aid in the diagnosis of a dissected aortic aneurysm.
If the carotid pulse is palpated for pulse contour and the femoral pulse for pulses paradoxus, then the radial pulse is palpated for rate and rhythm. The pulse rate and regularity are easily obtained here. The absence of a radial pulse should prompt a search for an ulnar pulse. An irregular pulse can be caused by atrial fibrillation; by premature beats arising in the atria, the atrioventricular junction, or the ventricles; and by second-degree atrioventricular block.
A slow, bounding hyperkinetic pulse can be found in complete heart block. Atrial Fibrillation causes an irregularly, irregular pulse. Not only will the rate of the pulse be irregular, but the pulse amplitude will also vary (Figure 17.6). This results from variable stroke volumes during systole. Note in Figure 17.6 how the systolic pressure varies from beat to beat. If the ventricular rate is rapid, some pulses may not be transmitted to the peripheral circulation. Simultaneous ausculation of the heart and palpation of the radial pulse can allow measurements of an apical to radial pulse deficit. Controlled atrial fibrillation should have no pulse deficit, that is, all central heartbeats are transmitted to the radial pulse and the peripheral circulation.
Figure 17.6
This aortic pressure pulse was recorded (scale of 0 to 200 mm Hg) in a patient with severe mitral regurgitation and atrial fibrillation. The peak systolic pressure varied from 80 mm Hg in the fourth beat to 110 mm Hg in the third and sixth beats. The (more...)
Figure 17.7
This aortic pressure tracing (scale of 0 to 200 mm Hg) was recorded in a patient who had coronary artery disease and a right coronary artery occlusion. The electrocardiogram shows premature ventricular beats (P) in bigeminy. The aortic pressure varies (more...)
- Marx HJ, Yu PN. Clinical examination of the arterial pulse. Prog Cardiovasc Dis. 1967;10:207–35. [PubMed: 4865412]
- O"Rourke MF, Avolio AP. Pulsatile flow and pressure in human systemic arteries. Circ Res. 1980;46:363–72. [PubMed: 6987005]
- O"Rourke RA. Physical examination of the arteries and veins. In: Hurst JW, ed. The heart, 6th ed. New York: McGraw-Hill, 1986:138–51.
- Smith JJ, Kampine JP. Pressure and flow in the arterial and venous systems. In: Circulatory physiology—the essentials. Baltimore: Williams and Wilkins, 1980; chap 4.
Figures
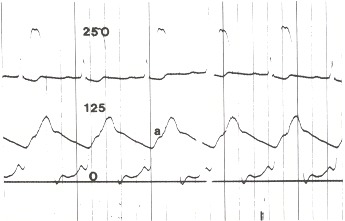
Figure 17.1
A simultaneous recording of left ventricular and aortic pressures in a patient with severe calcific aortic stenosis. The peak-to-peak pressure gradient is more than 125 mm Hg. Note the anacrotic notch (A) on the delayed upstroke of the aortic pulse.
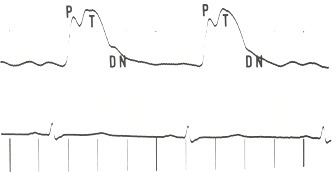
Figure 17.2
A carotid pulse tracing from a patient with severe aortic regurgitation. Note that the percussion wave (P) is smaller than the tidal wave (T), as it often is. Both percussion and tidal waves occur in systole before the dicrotic notch (DN).
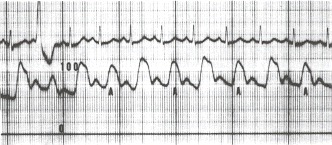
Figure 17.4
This aortic pressure tracing (scale of 0 to 100 mm Hg) was taken from a patient with a severe dilated idiopathic cardiomyopathy. The alternate pressure pulses (A) are 10 mm Hg lower than the pulses preceding them. Pulsus alternans was initiated by a premature ventricular beat.
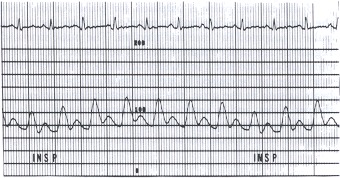
Figure 17.5
This aortic pressure pulse was recorded (scale of 0 to 200 mm Hg) in a patient with pericardial tamponade. During inspiration (INSP), the peak systolic pressure drops 20 mm Hg. The pulse rate was 120 beats per minute, and the respiratory rate was nearly 30 per minute. The arterial pressure varied from 120/80 to 100/70 mm Hg.
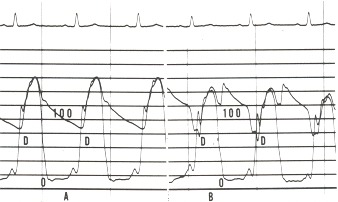
Figure 17.3
Panel A shows the simultaneous recording of the left ventricular and aortic pressures (on a scale of 0 to 200 mm Hg) in a patient with severe coronary artery disease. The aortic pressure is 160/90 mm Hg and the left ventricular end diastolic pressure is 22 mm Hg with a prominent A wave. In Panel B the intra-aortic balloon pump is generating a prominent diastolic wave. Note the aortic pressure has fallen to 140/80 mm Hg (D), and the left ventricular end diastolic pressure has fallen below 20 mm Hg.
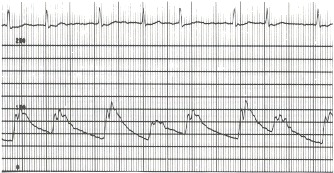
Figure 17.6
This aortic pressure pulse was recorded (scale of 0 to 200 mm Hg) in a patient with severe mitral regurgitation and atrial fibrillation. The peak systolic pressure varied from 80 mm Hg in the fourth beat to 110 mm Hg in the third and sixth beats. The patient also had a low cardiac output and pulmonary hypertension.
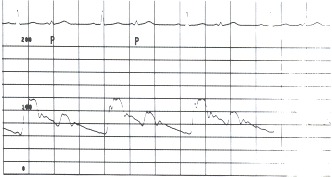
Figure 17.7
This aortic pressure tracing (scale of 0 to 200 mm Hg) was recorded in a patient who had coronary artery disease and a right coronary artery occlusion. The electrocardiogram shows premature ventricular beats (P) in bigeminy. The aortic pressure varies from 120/65 in the sinus beats to 100/80 in the premature beats.
Copyright © 1990, Butterworth Publishers, a division of Reed Publishing.
Không có nhận xét nào:
Đăng nhận xét