NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Bookshelf ID: NBK312 PMID: 21250154
Definition
The carotid pulse is characterized by a smooth, relatively rapid upstroke and a smooth, more gradual downstroke, interrupted only briefly at the pulse peak. These palpable pulsatile changes in the carotid arterial diameter are virtually identical to the intraluminal pressure pulse.Abnormalities of the carotid pulse may involve an alteration in the amplitude of the pulse peak, a distortion of the upstroke or downstroke, or any combination of these changes.
Technique
The carotid arterial pulses are usually examined with the patient supine and the trunk of the patient's body slightly elevated. The patient's chin should be elevated to allow easy palpation and yet not enough to tighten the neck muscles.During palpation of the pulse, the examiner uses the tactile or mechanoreceptors in the fingertips to sense movement of the arterial wall associated with the pressure pulse as it passes by the site of palpation. The fingers should be positioned between the larynx and the anterior border of the sternocleidomastoid muscle at the level of the cricoid cartilage. In palpating the pulse, the degree of pressure applied to the artery should be varied until the maximum pulsation is appreciated.
Opinions vary as to how many and which fingers should be used and as to the proper positional relationship between patient and examiner. Some physicians believe that tactile stimulus is accentuated by using a single finger and may even prefer to use the thumb. Others absolutely forbid use of the thumb for palpation and favor use of two or three fingers. Whichever finger or combination of fingers is used, it is essential that the examiner ascertain that he is not perceiving his own fingertip pulse. This potential error can be detected by pressing down with a finger at an adjacent body site not overlying the patient's artery. It is more likely that the examiner will perceive his own pulse if he uses his thumb. Generally, the carotid artery is palpated with the examiner sitting or standing comfortably at the patient's right side. Some clinicians, however, prefer to examine the carotid pulsations while standing at the head of the patient's bed. Because simultaneous palpation of the carotid artery and auscultation of the heart is occasionally beneficial, the examiner positioning himself at the patient's right side seems preferable.
Palpation of an arterial pulse may be directed toward assessing cardiac performance, determining cardiac rate and rhythm, establishing the integrity of the peripheral arterial blood supply, or localizing peripheral lesions. Examination of the carotid pulse is generally directed toward evaluating the status of the heart. While palpation of the carotid pulse is the most important component, the examination should also include inspection and auscultation. The absence of visible carotid pulsations suggest marked decrease in carotid pulse amplitude. The presence of a bruit may be a clue to partial carotid obstruction or may be a sound transmitted from a cardiac murmur.
Generally, the brachial artery is the preferable site for evaluating the condition of the patient's arterial walls. The hardness and tortuosity of the arterial wall can best be assessed at this site. The heart rate and rhythm are usually assessed by palpating the brachial or radial pulse.
Palpation of the carotid artery normally detects a smooth, fairly rapid outward movement beginning shortly after the first heart sound and cardiac apical impulse. The pulse peaks about one-third of the way through systole. This peak is sustained momentarily and is followed by a downstroke that is somewhat less rapid than the upstroke. Variations from this pattern may be noted during the upstroke, summit, or downstroke. The examiner's timing of the carotid pulse events may be improved by simultaneous auscultation of the heart. Palpation of the carotid pulse after a premature beat may be very helpful because certain pulse abnormalities are accentuated following a premature contraction.
Basic Science
The arterial pulse reflects the interaction between a driving force and impedance to blood flow. The driving force is dependent on the intrinsic contractility of the left ventricle, the size and shape of the heart, and the heart rate. The impedance is related primarily to peripheral resistance and arterial compliance associated with the distensibility of the vessel wall.The arterial pulse wave begins with opening of the aortic valve and ejection of blood from the left ventricle. The pressure pulse increases sharply as the blood enters the aorta faster than it flows to the periphery. The left ventricle ejects most of its stroke volume quite rapidly. A major portion of this rapidly ejected volume is transiently held in the proximal aorta and other large central arteries that are normally quite distensible. This rapidly rising portion of the carotid pressure curve is termed the anacrotic limb (anacrotic from the Greek "upbeat").
The height of pulse pressure is roughly proportional to the ratio of the stroke volume to arterial distensibility. Arterial distensibility, however, decreases as the distending pressure within the artery increases. Consequently, a given stroke volume will produce a larger pulse pressure if the mean arterial pressure is elevated. Arterial distensibility is also inversely related to the rate of rise of intraluminal pressure. As the rate of ventricular ejection accelerates, the arterial wall stiffens and the pulse pressure increases. The amplitude of the pulse pressure can also be modified by the "peripheral runoff." An accelerated runoff will lower the diastolic pressure and result in higher amplitude of the pulse pressure.
While the upstroke of the carotid pulse reflects the driving force and vessel compliance, the downstroke reflects the distensibility of vessels and the peripheral resistance. After the aortic pressure curve peaks, it begins a decline as ventricular ejection slows and blood continues to flow to the periphery. During the initial phase of ventricular relaxation, there is a momentary reversal of blood flow from the compliant central arteries back toward the ventricle. With this reversal of flow, the aortic valves close. A notch on the descending limb of the aortic pressure curve is associated with this transient reversal of blood flow. The subsequent smaller secondary positive wave, or dicrotic peak (dicrotic from the Greek "double beat"), has been attributed to the elastic recoil of the aorta and aortic valve. Following this small wave, the aortic pressure declines as peripheral runoff continues.
Clinical Significance
An inequality between the pulse amplitude in the two carotid arteries usually reflects atherosclerosis. Other possible explanations include aortic dissection, arteritis, or embolus. Kinking of the carotid artery is occasionally seen in a hypertensive patient and may simulate an aneurysm.The hyperkinetic pulse (Figure 20.1A) is characterized by an increase in the velocity of the upstroke and amplitude. The water-hammer, or Corrigan's, pulse is characterized by a very brisk upstroke, large amplitude, and rapid collapse; it is an extreme form of the hyperkinetic pulse. Hyperkinetic pulses may be associated with anxiety, exercise, fever, thyrotoxicosis, hypertension, aortic regurgitation, arterio-venous fistula, and patent ductus arteriosus. Patients with marked bradycardia may compensate with a large stroke volume clinically manifest by a hyperkinetic pulse. The water-hammer pulse is usually associated with aortic regurgitation.
The pulsus bisferiens (cf. Latin, "twice beating"), or bifid, arterial pulse is perceived as two narrowly separated positive waves during systole (Figure 20. 1B and 1C). The bifid pulse often occurs in patients with aortic regurgitation and is common in patients with combined aortic stenosis and aortic regurgitation. A similar pattern may occasionally be noted in other conditions characterized by a hyperkinetic pulse. The bifid pulse, as depicted in Figure 20.1C, is characteristic of idiopathic hypertrophic subaortic stenosis.
The hypokinetic arterial pulse (Figure 20.1D) is found in patients with a reduced stroke volume. This group includes patients with hypovolemia, left ventricular failure, and mitral stenosis.
A small and delayed arterial pulse, pulsus parvus et tardus (Figure 20.1E), is characteristic of severe valvular aortic stenosis. It must be recognized, however, that the absence of this finding, particularly in an elderly patient with noncompliant vasculature, does not exclude severe aortic stenosis.
Pulsus paradoxus is a characteristic pulse pattern in which there is marked attentuation in the amplitude of the pulse during the inspiratory phase of usual respiration. A paradoxical pulse must be measured with the sphygmomanometer and should be greater than 10 mm Hg to be significant. Pulsus paradoxus is common in pericardial tamponade but can also be seen with asthma, chronic obstructive airway disease, and superior vena cava obstruction.
Pulsus alternans is a beat-to-beat variation in the amplitude of the pressure pulse. It may be accentuated following a premature contraction. This pulse abnormality is usually best appreciated in distal arteries that have a wider pulse pressure than the carotid artery. Pulsus alternans is a manifestation of severe depression in left ventricular systolic function.
References
- Marx HJ, Yu PN. Clinical examination of the arterial pulse. Prog Cardiovasc Dis. 1967;10:207–35. [PubMed: 4865412]
- O"Rourke RA. Physical examination of the arteries and veins. In: Hurst JW, ed. The heart. New York: McGraw-Hill, 1982;188–93.
- Perloff JK. A modern view of an ancient art: feeling the pulse. GP. 1966;33:78–86.
- Tavel ME. Clinical phonocardiology and external pulse recording, 2d ed. Chicago: Year Book Medical Publishers, 1972.
Figures
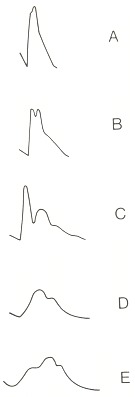
Figure 20.1
Carotid pulses: A, hyperkinetic pulse; B, bifid pulse; C, bifid pulse characteristic of IHSS; D, hypokinetic pulse; E, pulsus parvus et tardus.
Copyright © 1990, Butterworth Publishers, a division of Reed Publishing.
Không có nhận xét nào:
Đăng nhận xét